A Gates Foundation grant will help an Israeli scientist further develop his cell-phone imaging system for diagnosing and staging the serious African disease.

A simple mobile-phone imaging system developed in Israel for diagnosing and monitoring malaria has won its developers a $100,000 grant from the Bill and Melinda Gates Foundation.
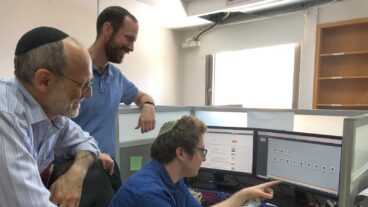
The grant is shared by biomedical engineer Dr. Alberto Bilenca of Ben-Gurion University of the Negev (BGU) and his research partner, Dr. Linnie Golightly of Weill Cornell Medical College in New York.
Now in the prototype phase, this new inexpensive weapon against Africa’s second-leading cause of death will be tested in the field in 2012. This will be a welcome advance in Africa, where the mosquito-borne disease causes an estimated 1,900 deaths every day in children under the age of five. This age group accounts for about 85 percent of malaria-related deaths.
Using an ordinary mobile phone camera with a $15 specialized lens, the system can detect malaria by imaging the eye or the skin to look for hemozoin, a pigment generated by the malaria parasite when it digests red blood cells. This pigment changes the orientation of light reflecting back from the tissue.
Significantly, the eye imaging also allows the system to determine the stage of the disease by measuring blood flow to the brain. Hemozoin blocks blood vessels and therefore slows the flow as greater amounts of it are released from the parasite. Monitoring blood flow in the brain is critical to checking the patient for cerebral malaria, the most serious form of the disease.
“Many devices are focused on diagnosis but not on monitoring the severity of the disease,” Bilenca explained. “We try to do both, because sometimes in villages of Africa you have to decide whether it is cost-effective to transport a child to the hospital, which is often a great distance away. We hope our device will help determine which patients need hospitalization, because it’s not possible to bring everyone who has malaria to the hospital.”
“Staging” the deadly disease is also critical to deciding the course of treatment.
Telemedicine possibilities
Another advantage of the cell phone device is that the images can be telecommunicated immediately to laboratories, in Africa and overseas, for diagnosis by experts. Researchers in Africa who lack sophisticated laboratory facilities depend on this method of data transmission.
Bilenca said the concept of detecting malaria through monitoring hemozoin was known for 30 years. “What’s new is that we are doing it with cell phones.”
The scientist joined the faculty of BGU in September last year from Harvard Medical School, and first developed the cell phone camera imaging system for measuring changes in blood flow, which is related to other conditions such as anemia and burns.
“I started to examine how blood flow is related to malaria, and realized we can do something there,” he said.
“To date, there are no means of diagnosing malaria and monitoring disease severity non-invasively by a low-cost, compact and easy-to-use device in field settings.”
Bilenca’s project received one of the 88 Gates Foundation grants awarded to researchers in 25 countries to support new initiatives for improving global health. This is the sixth round of funding from Grand Challenges Explorations (GCE), an initiative to help lower the barriers for testing innovative ideas in global health.