Prof. Smadar Cohen: We found that there is a high proliferation rate of cells in this area where the scaffold is implanted.One of the greatest roadblocks in helping heart attack victims fully recuperate and rehabilitate is the amount of heart tissue that dies as a result of the trauma – a condition that leaves the patients vulnerable to future heart failure. But this problem may be on its way to finding a solution, thanks to an Israeli research team.
The team recently created a biological “scaffold” that – in pigs – allows healthy injectable heart muscle cells to replace tissue that died as a result of a heart attack, through a process known as tissue engineering.
Successful clinical trials of this technique on human beings in the future could revolutionize the field of cardiology, providing physicians with the ability to cure heart-attack victims, helping them increase their life expectancy and improve their quality of life.
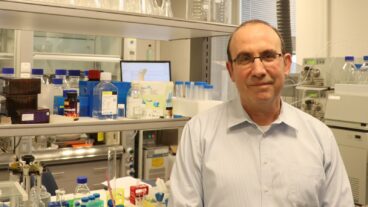
The research team was headed by Prof. Smadar Cohen of the department of biotechnology engineering, the department of medical engineering and the Institute for Applied Biosciences, at Ben-Gurion University of the Negev. Cohen’s team has just received an international patent for its pioneering technique of “scaffolding” the tissue.
The new “scaffold” – which functions as a template on which new cells are created, is non-toxic and does not activate the immune system. It is biologically and physiologically compatible with the human body and has enough durability for regenerating the tissue. After it does its job, the scaffold subsequently disintegrates in the body.
The polymer scaffold was originally developed as a tool to create cell cultures – a way to make human tissue outside of the body for experimentation, Cohen told ISRAEL21c.
But the more she worked with the scaffold and saw its effect on cells, she say, she noticed “exciting results. It began to look more and more as if the scaffold had healing properties,” she said, which inspired her team to begin its work with cardiac tissue.
This led her and her team to the work with cardial tissue. In the work with the pigs Cohen “found that new fibers grew into the scaffold, and we found that there is a high proliferation rate of cells in this area where the scaffold is implanted” and that “there is some kind of healing process and regeneration process in the heart.”
Working with Prof. Jonathan Leor from the Soroka Medical Center in Beersheba (and now at the Neufeld Cardiac Research Institute at Sheba Medical Center and Tel Aviv University), Cohen invented a polysaccharide (sugar) polymer scaffold to support transplanted cells, allowing them to survive, divide, organize themselves into a suitable structure and carry out their role as muscle tissue.
The scaffold the team created also encouraged the growth of capillaries to bring blood to the new tissue. Cohen, who recently presented her work at a biotechnology conference in Tel Aviv, said she and her team showed it effective on pigs.
The 10 pigs who suffered from congestive heart failure and were treated are all doing well, while there was a 40 percent mortality rate among the 10 pigs who were not treated. Cohen said they now have to work on larger numbers and prepare material for the US Food and Drug Administration.
With their research in advanced stages of experiments on young pigs, they hope the technology would be applied to human adult and embryonic stem-cell growth in the lab outside the body. Then, pieces of heart tissue could be grafted into the damaged heart and form on the template.
They are seeking several millions of dollars in financing from venture capital firms. With these funds, they plan to coordinate their animal work with FDA regulations and take steps towards trials and clinical studies for humans.
Aside from the breakthrough with heart tissue, the scaffolding technique shows great promise for other areas of medicine. The ability to “grow” human organ tissue using scaffolding would mean that the effects of new drugs or techniques on humans could be examined at an earlier stage of research, and would allow them to skip the controversial stages of medical research where many animals are sacrificed for experimentation.
Cohen finds it very exciting to be able to engineer human tissue outside the body “that can secrete and metabolize drugs just like the actual organ.” Currently, the team is also conducting research on other tissues, including the liver.
Cohen’s field of biotechnology engineering involves a uniquely interdisciplinary melding of engineering and medicine. Her background is in basic science, with a PhD in biochemistry and biophysics from Tel Aviv University, studies which involved computer simulations and models.
In 1992, looking for a way to apply her skills to a more immediate human application, she won the chance to do post-doctoral work with the renowned scientist Professor Robert Langer at MIT for work with biomaterials and polymers.
After five years at MIT, she declined other offers in order to return to Israel and join the faculty of Ben-Gurion University in order to establish her field in her native country, and found the university’s biotechnology engineering department.
She jokes that when she came from Cambridge “I went looking for the Charles River, and all I found was Nahal Beersheba. I continue to get offers but I love it at BGU,” she says. “We have a great dynamic program with the best students – these students could be going to the top medical schools, but have chosen biotechnology engineering instead.”