According to Prof. Jonathan Leor’s research, umbilical cord blood has turned out to be a very attractive source for myocardial repair.When Dr. Christian Barnard performed the world’s first successful heart transplant back in 1967, he reached a new peak of human scientific achievement.
However, almost 40 years later, the criteria for receiving a new heart is quite stringent, and heart transplants are granted to those patients who have the highest chance for recovery. For thousands of elderly or gravely ill patients with damaged hearts, a transplant is not an option.
Now Israeli researchers are at the forefront of research which could one day make heart transplants obsolete – using stem cell technology, they’re developing a way to use the blood of a newborn baby’s discarded umbilical cord (UCB) as an unlimited source of stem/progenitor cells that could be injected into the injured heart in order to regenerate damaged heart tissue.
Despite major advances in diagnosis and prevention, myocardial infarction (MI) continues to be a leading cause of morbidity and mortality around the world. According the American Heart Association, over 13 million Americans suffer from coronary heart disease, which account for over one million deaths a year.
The loss of heart muscle cells – or myocytes – in an injured heart often leads to irreversible deficits in cardiac function. Current clinical interventions to minimize the devastating effects of heart attack have not found a way to regenerate the damaged cells and prevent possible heart failure.
But recently, stem-cell based therapy has emerged as a novel strategy to repair
myocardial damage. However, according to Professor Jonathan Leor, one of the pioneers of the UCB research, one of the biggest unmet challenges so far has been to produce a sufficient number of suitable cells. He said that stem cell transplantation into the damaged tissue has limitations from both a practical and clinical points of view.
“The two main groups of stem cells that have been investigated until now as potential sources of tissue for repair are human embryonic stem cells and adult stem cells,” explained Leor, director of the Neufeld Cardiac Research Institute, a Tel-Aviv University Institute located at the Sheba Medical Center.
“The limitation of the former is that it’s difficult to control its differential – its conversion to adult tissue – and the risk of tumor formation is high. Another limitation is the likelihood of serious complications of immunosuppressive therapy – this could result in infections, or cancer,” Leor told ISRAEL21c.
“Adult stem cells on the other hand are autologous – they’re taken from the patient themselves, so they’re a perfect match. However, these stem cells are rare, and difficult to isolate. And if you’re dealing with a sick or elderly patient – which is mostly the case – their capacity of their cells to regenerate and proliferate is low,” he added.
For all those reasons, Leor said that there’s been a need to find alternative sources of stem cells for regeneration and repair. And, according to his research, umbilical cord blood has turned out to be a very attractive source for myocardial repair.
“UCB cells are readily available, are used in patients with hematologic disorders including genetic diseases and hematologic malignancies, and have many advantages that are relevant to cell therapy for cardiac healing and repair,” he said, adding, “The use of UCB stem cells is of importance to elderly and sick people in whom the availability of autologous stem cells is limited.”
Among the advantages he outlined are the UCB cells’ richness in stem and progenitor cells, with improved characteristics for regeneration. These cells can be easily obtained, expanded in vitro have the potential for enhanced self-renewal and can be ‘banked’ for future use.
The collection of UCB from as many donors as possible would also increase the likelihood of finding a match for people from many ethnic groups. And according to Leor’s research, it appears that there is reduced risk of rejection by the recipient’s immune system with UCB-derived stem cells. And finally, the use of UCB may make stem cell transplants available more quickly for patients with severe cases of heart disease who may die before a donor match can be made.
“The cells can participate in repair in more than one way – there’s the potential for them to be converted into heart cells or cells that create new vessels to repair the damaged heart tissue. In addition, the cells release molecules and hormones that promote the healing and repair of damaged heart cells,” he said.
Just as importantly, there is no ethical issue involved with using the stem cells of UCB, as there are with using stem cells from embryos.
“Usually, the umbilical cord is thrown away anyway, there’s no ethical dilemma involved, we’re not using an embryo,” said Leor.
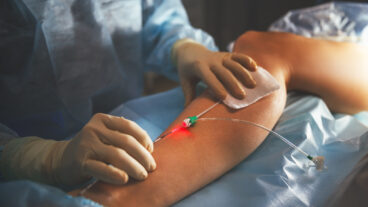
Leor – who worked together with Prof. Arnon Nagler, director of the Sheba Medical Center Hematology Department, its Bone Marrow Transplantation Unit, and its Cord Blood Bank, performed a pilot study to demonstrate the safety and feasibility of intracoronary delivery of UCB progenitor cells into the infarcted myocardium of pigs, and to track cell migration and colonization.
They discovered clusters of human cells had colonized and survived in the infracted myocardium – thus, the experiment proved that UCB-derived cells can be delivered to the infracted myocardium by a catheter-based technique and some cells can survive..
The mechanism by which cell transplantation improves cardiac function is uncertain and in many studies remains speculative, explained Leor.
“One of the challenges today is to develop a technique to expand the cells and increase their number,” he said, adding that he’s collaborating in this effort with Israeli stem cell research innovators Gamida-Cell in this effort.
Gamida-Cell is a leader in the expansion of blood stem cell therapeutics in clinical development for cancer and autoimmune diseases, as well as future regenerative cell-based medicines including cardiac and pancreatic repair.
“They have a patent on how to expand and increase the number of stem cells – we’re doing research for them. They’re expanding the cells, and we test them in animal model of heart disease. We have the proof of concept that even after expansion the cells are able to generate new tissue and improve heart function.” said Leor.
His team plans to initiate pre-clinical trials using pigs sometime before the end of the year.