‘Our message is that there’s a place for intervention in the very early stages of increased blood glucose levels – ranging from lifestyle modification, to possibly even drug intervention.’Blood sugar levels at the high end of ‘normal’ may not really be normal, according to a comprehensive Israeli research study. Coupled with other risk factors, the high end numbers may help identify apparently healthy men at increased risk of type 2 diabetes, who until now were given the clean bill of health, according to the study which was released last week in the prestigious New England Journal of Medicine.
Type 2 diabetes is the most common form of diabetes with millions of people afflicted. In people with type 2 diabetes, either the body doesn’t produce enough insulin – a hormone needed for the body to convert blood sugar to energy for cells – or the cells ignore the insulin. If left untreated, complications can include heart disease, blindness, and nerve and kidney damage, according to the American Diabetes Association.
Normal fasting blood sugar levels are considered those that fall below 99 milligrams per deciliter (mg/dl) of blood, while anything between 100 and 125 mg/dl is considered pre-diabetic, according to the National Institute for Diabetes and Digestive and Kidney Diseases. Once fasting glucose levels rise to 126 mg/dl and above, a person is considered diabetic. Fasting glucose levels are taken after a person hasn’t eaten for at least eight hours.
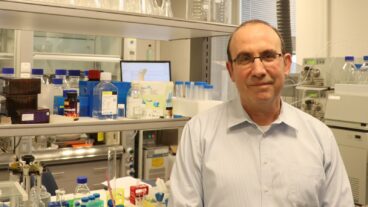
The Israeli study – a collaboration between Ben-Gurion University of the Negev, Sheba Medical Center and the Israel Defense Forces Medical Corp – suggests that more people may fall into the pre-diabetic category even if they have glucose levels at the high end of normal.
“What we found was that men with fasting blood glucose levels at the high end of normal – between 95 to 99 mg/dl – had about three times the risk of developing type 2 diabetes as men with blood sugar levels under 81 mg/dl,” said the study co-author Dr. Iris Shai, a researcher at BGU.
In the study, 13,000 healthy, non-diabetic male Israeli soldiers were followed over a multi-year period. The average follow-up time was 5.7 years. Besides the findings that showed that the men with blood glucose levels at the high end of normal more likely to develop diabetes, the study showed that men who had additional risk factors and high-normal blood glucose readings were even more likely to develop type 2 diabetes.
“If you combine those high end levels with other factors like obesity or high triglycerides, the risk is even higher,” Shai told ISRAEL21c.
For example, obese men with fasting glucose levels between 91 and 99 mg/dl had eight times the risk of developing the disease, compared to non-obese men with blood glucose readings less than 86 mg/dl, the study found.
“The question we were trying to answer is whether a normal blood glucose count among apparently healthy young men can predict future diabetes,” said Shai.
What they concluded was that higher fasting plasma glucose levels within the normal range constitute an independent risk factor for type 2 diabetes among young men, and such levels may help, along with body-mass index and triglyceride levels, to identify apparently healthy men at increased risk for diabetes.
“The results suggest that a normal glucose level (a level that is not associated with increased diabetes risk) may have to be defined in a more individualized manner with different values, depending on a person’s additional risk factors,” study co-author Dr. Amir Tirosh told HealthDay News.
“The novelty of this study is that it was conducted among a distinct population of relatively young, healthy men. What we found out is that perhaps the cut point of what constitutes ‘normal’ should be considered differently for different populations, especially when combined with obesity and high triglycerides,” added Shai.
“Doctors may test the glucose level and find it normal, but it’s a question of definition. The normal of yesterday is not necessarily the normal of today.”
The findings could have implications for determining when to treat people at risk with blood sugar-lowering medications. Both Shai and Tirosh recommended changing the way both physicians and patients relate to the numbers.
“Our message is that there’s a place for intervention in the very early stages of increased blood glucose levels – ranging from lifestyle modification, to possibly even drug intervention,” said Shai who recently returned to Israel after spending two years at Harvard.
She added that while women were not included in the study, it was logical to extrapolate that the conclusions would be similar.
“People and physicians should not look only on the current definition of normal and abnormal blood glucose levels when assessing an individual’s risk to develop diabetes. A careful interpretation of the body mass index, the triglyceride level and the patient’s family history of diabetes is needed in order to better identify those at high risk,” added Tirosh, an internist and researcher at the department of internal medicine at Sheba Medical Center.
Diabetes specialist Ronald Arky, MD, of Harvard Medical School, in an editorial accompanying the study in the same issue of the NEJM wrote that “blood glucose means very little if you don’t considered obesity, sedentary lifestyle, smoking, family history, and other diabetes risk factors along with it.”
Arky wrote that the lessons learned about cholesterol and cardiovascular disease can help guide doctors in better understanding blood sugar and diabetes. Revised guidelines released just over a year ago lower target cholesterol levels, but only for patients with the greatest risk of having a heart attack or stroke. The new research shows that the same individualized approach is called for when counseling patients about their diabetes risk, Arky and Tirosh told the WebMD web site.
“We know what the risks are,” Tirosh says. “By better recognizing them we may be able to prevent or at least delay diabetes with lifestyle modification and drug therapy.”