The patients would go out for walks with the dog, have discussions about caring for the animal and other issues related to the pet.It may be conventional wisdom that a dog is a man’s best friend, but researchers in Israel are providing another reason to salute our canine companions.
Undergoing psychosocial therapy with a dog present as the focus can help people with schizophrenia feel more motivated and improve their quality of life, a team from the Technion Institute of Technology in Haifa and the Sha’ar Menashe Mental Health Center near Hadera have shown.
In a study published in the journal Psychotherapy and Psychosomatics, the team presented encouraging results from their investigation into the effect of bringing dogs into therapy sessions.
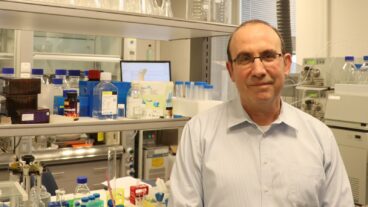
According to the supervisor of the study, Professor Henry Silver, the researchers found was that patients in these sessions were much less apathetic compared to those who underwent conventional therapy.
Silver, deputy director of medical center, and member of the Rappaport Faculty of Medicine at at the Technion, supervised the graduate work of Inbar Nathans-Barel, and devised the idea for the study.
“Inbar was an animal trainer during her army service, and she was interested in applying the method in clinical field. Since I have been researching novel treatments for persons suffering from schizophrenia we decided to investigate use this method,” Silver told ISRAEL21c.
The research team looked at anhedonia, the inability to gain pleasure from normally pleasurable experiences, which is a major factor in schizophrenia. For example, an anhedonic mother gains no joy from playing with her baby, a sports fan is no longer excited when his team wins and a teenager is left unmoved by listening to his favorite music. The condition is linked to poor social functioning and has proved resistant to treatment, said Silver, who is originally from Australia and immigrated to Israel in 1980.
“We work a lot on the issue of emotional processing in schizophrenia patients, and utilize various training methods. We especially look at negative symptoms in a patient – the lack of normal personality features, apathy, and lack of interest that are particularly affected by the illness. These present a major obstacle to rehabilitation,” he said. “In this particular study, it was in the context of trying see if adding the presence of an animal in therapy session would have a positive impact.”
The researchers compared 10 schizophrenia patients who underwent animal-assisted therapy and 10 who were given non-animal-assisted therapy over a 10 week period.
“We set up a controlled study – with patients who had been hospitalized for some time with severe problems with apathy and ability to conduct social relations. In one group the patients had weekly one hour sessions over a 10 week period with Inbar and a dog she brought to the sessions.
“The dog was trained not to approach the patients directly, but respond to their initiatives. It was a program designed to encourage interaction with the animal and discussion about the interactions. The patients would go out for walks with the dog, have discussions about caring for the animal and other issues related to the pet,” said Silver.
Patients in the other group had the same 10-week sessions with the same therapist, but without the dog. There was similar content however – in the sessions, they discussed caring for the pet, going for walks – in an attempt to present as controlled a situation as possible, he explained.
In both groups, the researchers assessed patients’ clinical symptoms, their subjective views of their quality of life and their hedonic tone – a psychological term relating to whether someone views experiences as pleasurable.
“After the first five weeks, there was an improvement in both groups in the patients’ ability to interact and their motivation. This is a normal reaction to a new situation in which somebody comes and talks to them, and gets them to talk,” said Silver. “But if you go on, the group without the dog plateaued after the first five weeks, while the group with the dog continued to improve, leaving quite a big difference between the behavior of the two groups.”
The group who were given pet therapy showed a significant improvement in the hedonic tone compared to the other group. They were also seen to show an improvement in the use of leisure time and a trend towards improvement in motivation. According to Silver, the group with the dog was motivated in a number of various ways.
“It was quite a significant change – they would actually look forward to the sessions. Usually, these patients interact poorly with people, they’re often disheveled, they’re resistant to bathing. But once they began their weekly meeting with the dog, they began to change. One woman who previously had to be forced to shower, was now getting ready herself. ‘The dog will get offended if I don’t look good’ she told us.”
After the 10 sessions, Silver explained that there were two separation sessions with the group ? in order to help them deal with lessening their attachment to the dog.
“They were able to talk about issues like taking care of the dog if it was sick – which was qualitatively different for them. Often they don’t show an interest in others. They expressed that they would miss seeing the dog – and these are people who wouldn’t care if their families came to visit them or not.
Silver hopes to conduct another enlarged study, if he can obtain the funding, but he says that the study has already had a major benefit.
“What we’ve learned is that this may offer an additional means of treating an area of schizophrenia which has been resistant to every sort of treatment. Even patients that are deemed recovered often don’t regain their sense of social contact, and motivation.”
According to the team’s written study, animal-assisted therapy “may contribute to the psychosocial rehabilitation and quality of life of chronic schizophrenia patients.”
“We’d like to look at the potential mechanism at the bio chemical and the cognitive levels,” said Silver. “One piece of the puzzle is trying to understand the mechanism of the pathology in schizophrenia and how we can help. There are pharmacological methods which can help, and now there are a number of non-pharmacological methods like this.”